Items filtered by date: May 2024
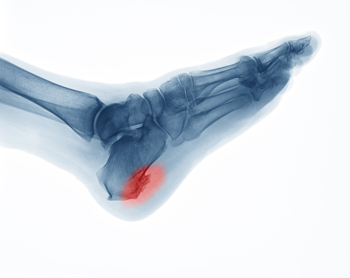
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
When Surgery Is Needed for Heel Spurs
When conservative treatments prove ineffective in easing the discomfort, inflammation, and swelling associated with heel spurs, surgery emerges as a viable solution. These outgrowths on the heel bone, medically termed calcaneal spurs, can cause significant pain and impede mobility. The decision to pursue surgery hinges not solely on the size or presence of the spur, but rather on the persistence of pain resistant to treatment. Podiatrists typically advocate for surgery when symptoms persist despite six months of non-surgical interventions. Two primary approaches exist for heel spur surgery, which are known as open surgery and endoscopic surgery. Open surgery entails larger incisions and is generally employed to excise entire spurs. Endoscopic surgery employs smaller incisions, fostering quicker recovery and fewer complications. The surgical procedure may vary depending on the spur's location, whether it is inferior or posterior. Inferior heel spurs often coexist with plantar fasciitis and are addressed through plantar fasciotomy. Posterior heel spurs near the Achilles tendon may necessitate more intricate procedures, especially if the spur is deeply embedded within the Achilles tendon. While heel spur surgery has a high success rate, it also carries risks of nerve injury, foot instability, and acquired flat feet. If you are in pain from a heel spur, it is suggested that you consult a podiatrist who can determine what the best course of treatment is for you.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Shawn Echard, DPM from Laurel Podiatry LLC. Our practitioner will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Greensburg and Somerset, PA . We offer the latest in diagnostic and treatment technology to meet your needs.
What Are Hammertoes?
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a physician—particularly a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions of your doctor is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.
Diagnosis and Causes of Hammertoe

Hammertoe, a condition affecting the toes, manifests as an abnormal bend in one or more joints, resembling a hammer's shape. This deformity typically occurs in the second, third, or fourth toe, leading to discomfort and difficulty while wearing shoes. Causes of hammertoe vary, with prominent factors including prolonged wearing of ill-fitting footwear, toe injuries, muscle imbalance, and conditions like arthritis. Diagnosing hammertoe involves a physical examination by a podiatrist, who assesses the toe's flexibility, alignment, and range of motion. Additionally, X-rays may be performed to confirm the diagnosis and evaluate the severity of the deformity. Early detection is essential, as untreated hammertoe can worsen over time, leading to chronic pain and mobility issues. Once diagnosed, treatment options may include orthotic devices, toe exercises, shoe modifications, and in severe cases, surgery to correct the toe's alignment. If you have a hammertoe, it is strongly suggested that you consult a podiatrist who can determine the best course of treatment for you.
Hammertoe
Hammertoes can be a painful condition to live with. For more information, contact Shawn Echard, DPM from Laurel Podiatry LLC. Our practitioner will answer any of your foot- and ankle-related questions.
Hammertoe is a foot deformity that affects the joints of the second, third, fourth, or fifth toes of your feet. It is a painful foot condition in which these toes curl and arch up, which can often lead to pain when wearing footwear.
Symptoms
- Pain in the affected toes
- Development of corns or calluses due to friction
- Inflammation
- Redness
- Contracture of the toes
Causes
Genetics – People who are genetically predisposed to hammertoe are often more susceptible
Arthritis – Because arthritis affects the joints in your toes, further deformities stemming from arthritis can occur
Trauma – Direct trauma to the toes could potentially lead to hammertoe
Ill-fitting shoes – Undue pressure on the front of the toes from ill-fitting shoes can potentially lead to the development of hammertoe
Treatment
Orthotics – Custom made inserts can be used to help relieve pressure placed on the toes and therefore relieve some of the pain associated with it
Medications – Oral medications such as anti-inflammatories or NSAIDs could be used to treat the pain and inflammation hammertoes causes. Injections of corticosteroids are also sometimes used
Surgery – In more severe cases where the hammertoes have become more rigid, foot surgery is a potential option
If you have any questions please contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.
Surfing Foot and Ankle Injuries

Wind, wave, and kite surfing offer exhilarating experiences, but they also pose risks of foot and ankle injuries. Collisions with the board, submerged obstacles near the shore, or rotation trauma with the foot secured in straps are common culprits. Reef cuts and open wounds, prevalent in tropical waters, can lead to severe infections. Among the array of potential injuries, midfoot injuries are particularly concerning and often result in chronic instability and arthritis if not properly addressed. Additionally, falls with the foot trapped in straps necessitate examination for Lisfranc joint lesions and subtalar injuries. A podiatrist can help to manage these injuries. Podiatrists can accurately diagnose conditions, offer tailored treatment plans, and provide rehabilitation strategies to promote optimal healing and prevent long-term complications. If you have sustained an injury from surfing, it is suggested that you schedule an appointment with a podiatrist who can help restore your foot and ankle function.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with Shawn Echard, DPM from Laurel Podiatry LLC. Our practitioner will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions, please feel free to contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
Custom Orthotics Prescribed for Adults and Kids

Orthotics are invaluable tools for both adults and children in addressing a range of foot conditions and promoting optimal foot function. Podiatrists often prescribe orthotics to correct rearfoot positioning, providing stability and alignment. Certain types of orthotics, such as custom-made rigid or semi-rigid orthotics, consistently yield successful outcomes by offering durable support and control over foot motion. Effectiveness is assessed by podiatrists through careful evaluation of gait patterns, foot structure, and symptom improvement over time. Orthotics should be replaced periodically to ensure continued effectiveness, typically every one to three years depending on usage and wear. Regular follow-up appointments with a podiatrist are essential to monitor foot health and make any necessary adjustments to orthotic prescriptions. By utilizing orthotics tailored to individual needs and regularly assessing their efficacy, both adults and children can experience improved comfort, function, and mobility in their daily lives. If you or your child have foot problems, it is suggested that you schedule an appointment with a podiatrist to discuss whether custom made orthotics can help you.
Experience a transformative solution to heel pain and foot pain through the personalized benefits of custom orthotics and shoe inserts. If you’re grappling with the persistent agony of plantar fasciitis, these customized inserts are designed to alleviate the strain on the plantar fascia, providing targeted relief. Engineered to adapt to your unique foot anatomy, custom orthotics tackle not only plantar fasciitis but also general foot and heel pain, offering unparalleled support and comfort. Don’t let every step be a reminder of discomfort; step into a world of tailored well-being. Say farewell to the limitations imposed by heel pain and embrace the freedom of pain-free mobility. Invest in your foot health and redefine your daily stride with the transformative power of custom orthotics and shoe inserts, ensuring each step is a step towards lasting comfort.
If you have any questions please contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Broken Ankle
Broken ankles or “ankle fractures” are injuries that occur when the bones that make up the ankle joint are broken. Ankle injuries are some of the most common bone and joint injuries. The ankle joint is made up of three bones that join. The tibia is the main bone, and it makes up the inside of the anklebone. The fibula is a smaller bone, and it makes up the outside of the anklebone. A membrane called the joint capsule is lined with a layer called the synovium, which covers the entire joint. The synovium produces synovial fluid which allows for the joint surfaces to move.
An ankle becomes broken when the joint is stressed beyond the strength of its limits. When an ankle is fractured, ligaments may also tear at the same time. Fractures often occur to the ankle rolling or twisting in an unusual way. At times, a fracture may even be caused by an extreme force applied to the joint.
Symptoms of a broken ankle include pain, swelling, bruising, discoloration, numbness, and an inability to move the toes. If you have a broken ankle, you may also hear something tear or snap when you initially suffered the injury. If you have pain from a broken ankle, beware that the pain will not always come from the exact area of the fracture; you may also experience pain from associated foot fractures. The swelling you may experience can suggest that soft tissue damage may have occurred due to the injury.
There are differences between an ankle fracture and an ankle sprain. The difference is that a fracture or break in the bone is required to classify an injury as a broken ankle. An ankle sprain occurs when there is a tear or disruption of ligaments in the ankle. In some cases, the prognosis of an ankle sprain may be worse than that of a fracture.
X-rays are the most common way to diagnose a broken ankle. X-rays show if the ankle is broken and where exactly the fracture is located. It will also show how many pieces of broken bone there are. A second method of testing to see if an ankle is broken is a stress test. To do this, the doctor will put pressure on the ankle and perform a stress test to determine if the fracture requires surgery. Other methods for diagnosis include CT scans and MRI scans.
If you are suffering from a broken ankle, consult with your podiatrist immediately to receive a proper diagnosis and treatment.
Ankle Fracture Care

A broken ankle occurs when the bones forming the ankle joint suffer fractures. This injury often arises from sudden impacts, twists, or repetitive stress on the ankle. Symptoms typically entail intense pain, swelling, bruising, difficulty walking, and potential deformity surrounding the ankle area. Managing a broken ankle depends on factors like the extent and location of the fracture. Treatment options may include immobilization using a cast or splint, rest, elevation, and occasionally surgical intervention to realign and stabilize the bones. If you have broken your ankle, it is suggested that you schedule an appointment with a podiatrist who can offer specialized expertise in diagnosing and treating foot and ankle conditions, including fractures.
Broken ankles need immediate treatment. If you are seeking treatment, contact Shawn Echard, DPM from Laurel Podiatry LLC. Our practitioner can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
