Blog
Causes of an Infected Foot Blister

An infected foot blister develops when a fluid filled lesion on the skin becomes contaminated with bacteria, often after friction, pressure, or improper care. Blisters commonly form from wearing tight footwear, prolonged walking, or moisture that irritates the skin. When infection occurs, symptoms may include increased pain, redness, warmth, swelling, foul smell, and the presence of pus. The surrounding skin may feel tender and appear inflamed, making walking uncomfortable. Relief options include keeping the area clean, protected, and properly dressed to reduce further irritation. A podiatrist can evaluate the severity of the infection, provide appropriate treatment to prevent complications. If you have a foot blister that has become infected, it is suggested that you consult a podiatrist who can offer effective treatment and prevention solutions.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Shawn Echard, DPM of Laurel Podiatry LLC. Our practitioner can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Myofascial Release and Its Benefits for Mobility

Foot myofascial release is a technique designed to relieve tension within the myofascia, which is connective tissue that supports the muscles and structures of the foot. This method can be performed by rolling the sole of the foot over a tennis ball while applying comfortable pressure. The movement helps mobilize toe joints, hydrate connective tissue, and stimulate nerve endings that support proper function. Regular practice may reduce stiffness, improve circulation, and enhance overall balance by promoting better foot mobility and stability. It can also ease discomfort associated with prolonged standing or activity. A podiatrist can demonstrate proper technique and evaluate underlying concerns. If you have foot pain, it is suggested that you consult a podiatrist who can determine the type of treatment you need, which may include stretches.
Why Stretching Is Important for Your Feet
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Shawn Echard, DPM from Laurel Podiatry LLC. Our practitioner will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Stretching the muscles in the foot is an important part in any physical activity. Feet that are tight can lead to less flexibility and make you more prone to injury. One of the most common forms of foot pain, plantar fasciitis, can be stretched out to help ease the pain. Stretching can not only ease pain from plantar fasciitis but also prevent it as well. However, it is important to see a podiatrist first to determine if stretching is right for you. Podiatrists can also recommend other ways to stretch your feet. Once you know whether stretching is right for you, here are some excellent stretches you can do.
- Using a foam roller or any cylindrical object (a water bottle or soda can will do), roll the object under your foot back and forth. You should also exert pressure on the object. Be sure to do this to both feet for a minute. Do this exercise three times each.
- Similar to the previous exercise, take a ball, such as a tennis ball, and roll it under your foot while seated and exert pressure on it.
- Grab a resistance band or towel and take a seat. If you are using a towel, fold it length wise. Next put either one between the ball of your foot and heel and pull with both hands on each side towards you. Hold this for 15 seconds and then switch feet. Do this three times for each foot.
- Finally hold your big toe while crossing one leg over the other. Pull the toe towards you and hold for 15 seconds. Once again do this three times per foot.
It is best to go easy when first stretching your foot and work your way up. If your foot starts hurting, stop exercising to ice and rest the foot. It is advised that you then see a podiatrist for help.
If you have any questions please contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
When Swelling in the Feet Tells a Bigger Story

Swelling of the feet occurs when excess fluid builds up in the tissues. It is often linked to underlying medical conditions, circulation problems, prolonged standing, or pregnancy. Symptoms include puffiness, tight skin, aching, and a heavy sensation that worsens as the day goes on. The feet may look enlarged or shiny, and pressing on the skin can leave a temporary indentation. This swelling can feel uncomfortable or painful and may limit movement or make shoes feel tight. A podiatrist can help by beginning with a thorough evaluation to determine the cause, including reviewing medical history and ordering imaging or other tests when needed. Treatment may focus on reducing fluid buildup through lifestyle guidance, compression support, and targeted exercises to improve circulation. Ongoing care helps protect skin health and prevent complications. If you have swelling of the feet, it is suggested that you make an appointment with a podiatrist.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact Shawn Echard, DPM of Laurel Podiatry LLC. Our practitioner can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Growing Feet and Aching Heels
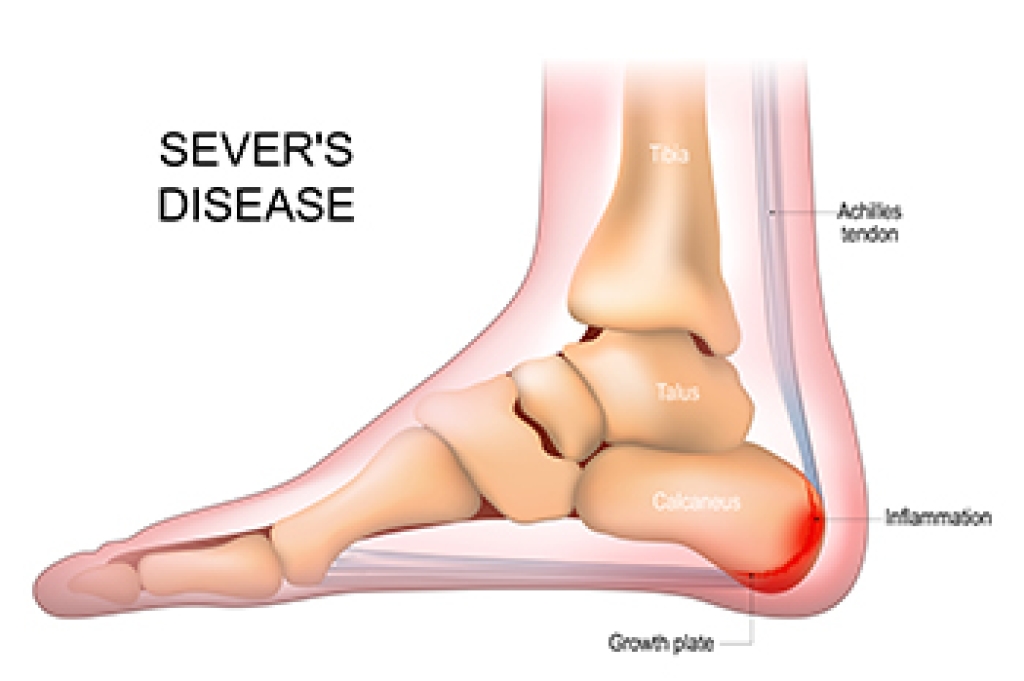
Sever's disease is a common cause of heel pain in active children, particularly during growth spurts when the heel bone develops faster than the surrounding soft tissues. Symptoms include limping after sports, avoiding pressure on the heel, or walking on their toes to reduce discomfort. It may feel like a sharp ache at the back of the heel that worsens with running or jumping. The condition is usually caused by repetitive stress on the heel growth plate, tight calf muscles, or sudden increases in activity. Helpful stretches include the soleus stretch, which gently lengthens the lower calf, and heel dips, which improve flexibility and reduce strain on the heel. A podiatrist can assist from the start by providing a clear diagnosis, assessing foot structure, and recommending personalized treatments. Among them are activity modification, stretching programs, supportive footwear, and orthotic devices. If your active child is experiencing heel pain, it is suggested that you make an appointment with a podiatrist.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Shawn Echard, DPM from Laurel Podiatry LLC. Our practitioner can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Greensburg and Somerset, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.